- Severe bleeding
- A hole in the colon (perforated colon)
- Severe dehydration
- Bone loss (osteoporosis)
- Inflammation of your skin, joints and eyes
- An increased risk of colon cancer
- A rapidly swelling colon (toxic megacolon)
- Increased risk of blood clots in veins and arteries
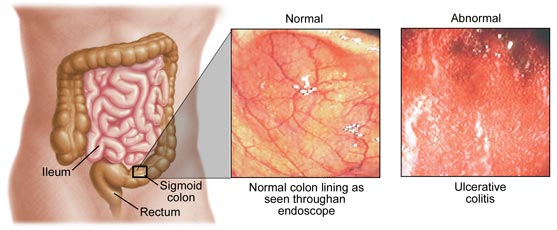
Patients with ulcerative colitis limited to the rectum (proctitis) or colitis limited to the end of the left colon (proctosigmoiditis) usually do quite well. Brief periodic treatments using oral medications or enemas may be sufficient. Serious complications are rare in these patients. In those with more extensive disease, blood loss from the inflamed intestines can lead to anemia and may require treatment with iron supplements or even blood transfusions. Rarely, the colon can acutely dilate to a large size when the inflammation becomes very severe. This condition is called toxic megacolon. Patients with toxic megacolon are extremely ill with fever, abdominal pain and distention, dehydration, and malnutrition. Unless the patient improves rapidly with medication, surgery usually is necessary to prevent colon rupture.
Colon cancer is a recognized complication of chronic ulcerative colitis. The risk for cancer begins to rise after eight to ten years of colitis. Patients with only ulcerative proctitis probably do not have increased risk of colon cancer compared to the general population. Among patients with active pancolitis (involving the entire colon) for 10 years or longer, the risk of colon cancer is increased compared to the general population. In patients with colitis limited to the left side of the colon, the risk of colon cancer is increased but not as high as in patients with chronic pancolitis.
The current estimates for the cumulative incidence of colon cancer associated with ulcerative colitis are 2.5% at 10 years, 7.6% at 30 years, and 10.8% at 50 years. Patients at higher risk of cancer are patients with positive family histories of colon cancer, long durations of colitis, extensive colon involvement, and primary sclerosing cholangitis (PSC), another complication of ulcerative colitis.
Since these cancers have a more favorable outcome when diagnosed and treated at an earlier stage, yearly colon examinations may be recommended after eight years of known extensive disease. During these examinations, samples of tissue (biopsies) can be taken to search for precancerous changes in the lining cells of the colon. When precancerous changes are found, removal of the colon may be necessary to prevent colon cancer.
Complications of ulcerative colitis can involve other parts of the body. Ten percent of the patients can develop inflammation of the joints (arthritis). Some patients have low back pain due to arthritis of the sacroiliac joints. Rarely, patients may develop painful, red, skin nodules (erythema nodosum).
Yet others can have painful, red eyes (uveitis, episcleritis). Because these particular complications can risk permanent vision impairment, eye pain or redness are symptoms that require a physician's evaluation. Diseases of the liver and bile ducts may also be associated with ulcerative colitis. For example, in rare patients with a condition called sclerosing cholangitis, repeated infections and inflammation in the bile ducts can lead to recurrent fever, yellowing of skin (jaundice), cirrhosis, and the need for a liver transplant.